Speech Therapy, The Department of Rehabilitation
Speech Therapy
Two Speech Therapists (ST) provide examination, training, and other assistance to adults who have problems with speech and swallowing due to stroke or traumatic brain injury.Speech and Language Disorders
There are three main types of language disorders after stroke or traumatic brain injury: aphasia, dysarthria, eating and swallowing dysfunction, and communication disorders associated with generalized mental inactivity. Although these disorders may occur in combination, they are distinguished in the following waysAphasia
- A condition in which a person is unable to name things correctly or mishear what others are saying due to damage sustained in the language area of the brain.
- The patient is intellectually intact but has difficulty in speaking, listening, reading, writing, and calculating.
- Symptoms and severity vary, such as not being able to speak a single word or speaking gibberish that one does not understand.
Dysarthria
- A disorder of the nerves that move the lips, tongue, and vocal cords, causing problems such as difficulty moving the lips and tongue, slurred speech due to lack of articulation, and difficulty communicating speech.
- Communication functions such as “listening,” “reading,” and “writing” are maintained, and communication is possible through nodding/neck shaking, written communication, etc.
Eating and swallowing dysfunction
- Due to paralysis of the lips and tongue, drooling, chewing and swallowing food may also be impaired.
Communication disorders associated with generalized mental inactivity
- More likely to occur after extensive brain damage or repeated strokes.
- The patient lacks motivation to speak, does not respond to questions, closes his eyes, or does not smile.
- The patient also lacks motivation in daily life.
About Training
Based on the results of the examination, we explain the speech symptoms to the patient and his/her family. We will also formulate a plan for the future, and aim to improve communication skills through individual training in the inpatient and outpatient settings. If necessary, we will work with doctors, caseworkers, and other rehabilitation staff to assist the patient in returning to work or living after discharge. Furthermore, for those who continue to need assistance after completion of certain training, we refer them to welfare facilities, friendship groups, and other places where they can obtain communication opportunities suited to their needs. We also provide consultation for language disorders other than aphasia, dysarthria, eating and swallowing dysfunction, communication disorders associated with generalized mental inactivity, or higher brain dysfunction other than language.Eating and Swallowing Dysfunctions
The process of swallowing food through the mouth is divided into the following six stages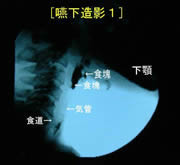
Even after swallowing, a part of the food mass remains in the hollow of the throat (epiglottis valley) even after swallowing.
- Recognition of food (awake and aware of the need to eat)
- Ingestion into the mouth (lips open to take in food, then lips closed to hold)
- Chewing and food lump formation (chewing well and mixing with saliva to form a lump that is easy to swallow)
- Sending to pharynx (food is sent to the back of the mouth by tongue movement)
- Passage through the pharynx and into the esophagus (the swallowing reflex sends the food mass into the esophagus)
- Passage through the esophagus (peristalsis of the esophagus sends a food mass to the stomach)
When the nerves of the mouth and throat are damaged due to stroke or other causes, problems mainly occur in stages 2-5. It is difficult to obtain accurate information about these processes from external observation alone, especially the presence or absence of aspiration (food accidentally entering the trachea), which is the most important of all.
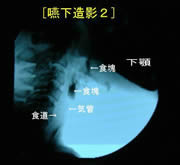
At the moment of swallowing, a part of the food mass into the airway at the moment of swallowing (laryngeal intrusion/aspiration).
The doctor in charge of the patient performs a swallow angiogram (an x-ray that shows how the patient swallows food), and based on the results of the angiogram, the patient’s doctor formulates a plan to provide training in a safe and effective manner.
The ST plays a central role in indirect swallowing training (training without food), including exercise training of the oral organs.
In direct swallowing training using swallowing training foods such as jelly, various problems such as body position, food form, and the patient’s preferences are discussed with doctors, nurses, physical therapists, occupational therapists, dietitians, and other staff members to help the patient regain the joy of eating by mouth.